The Healthcare Divide: Quaternary vs Government Hospitals in India
The evolving technology will change the medical landscape pretty soon. Can't guarantee these innovations would reach masses but if you are a HNI you might access them at a top tier private hospital.
Hospitals are of 4 tiers based on the location, services and sophistication of procedures offered. From lowest to highest tier, they are primary, secondary, tertiary and quaternary hospitals. India's healthcare system is traditionally structured into three tiers: Primary, Secondary, and Tertiary care. Quaternary care is an extension of tertiary care, involving highly specialized and experimental treatments.(1,2,3)
Quaternary care is the highest tier of all and mostly a last resort for patients(similar to supreme court) to get treated for severe and rare medical conditions that often need specialised, often experimental treatment. However, quaternary care hospitals are extremely expensive, making them impractical for treating large populations due to their high operational costs. As a result, tertiary, secondary and primary hospitals play a vital role in managing minor conditions while referring the more severe cases to higher-tier facilities. This article compares and contrasts the operation of private-run quaternary hospitals and government-run hospitals in India.
Introduction to a Quaternary Hospital: A Walk Through
When I enter a quaternary hospital(the top-tier facility) it’s stepping into another world. The place is huge, well lit— not too bright nor too dim, just right for a patient’s eyes, with spacious corridors, waiting areas and well maintained wards with beds to accomodate a large influx of patients. Each specialist has a separate consultation cabin, and each floor is dedicated to a specific organ system. The quaternary hospital, mostly is a single building that is well connected to facilitate patients to move from one department to another, thanks to numerous elevators. A round-the-clock emergency department, combined with an advanced diagnostics unit offering a full range of medical tests, enables rapid diagnosis and timely treatment of critical emergencies. The entire experience feels fast-paced from booking appointment to taking consultation, getting tests done in hours to getting those tests reviewed, getting appointment for a procedure to getting that procedure done asap.
The experience feels like water flowing down a stream—smooth and efficient, so is the money from the wallet.
I have to be ready to spend a hefty amount out-of-pocket on top of my insurance cover(assuming I have one) if I were to be admitted in a quaternary hospital for a severe illness. Private quaternary hospitals are in the business of making a profit, and treatment costs reflect that.
Unboxing the Government Hospital Experience
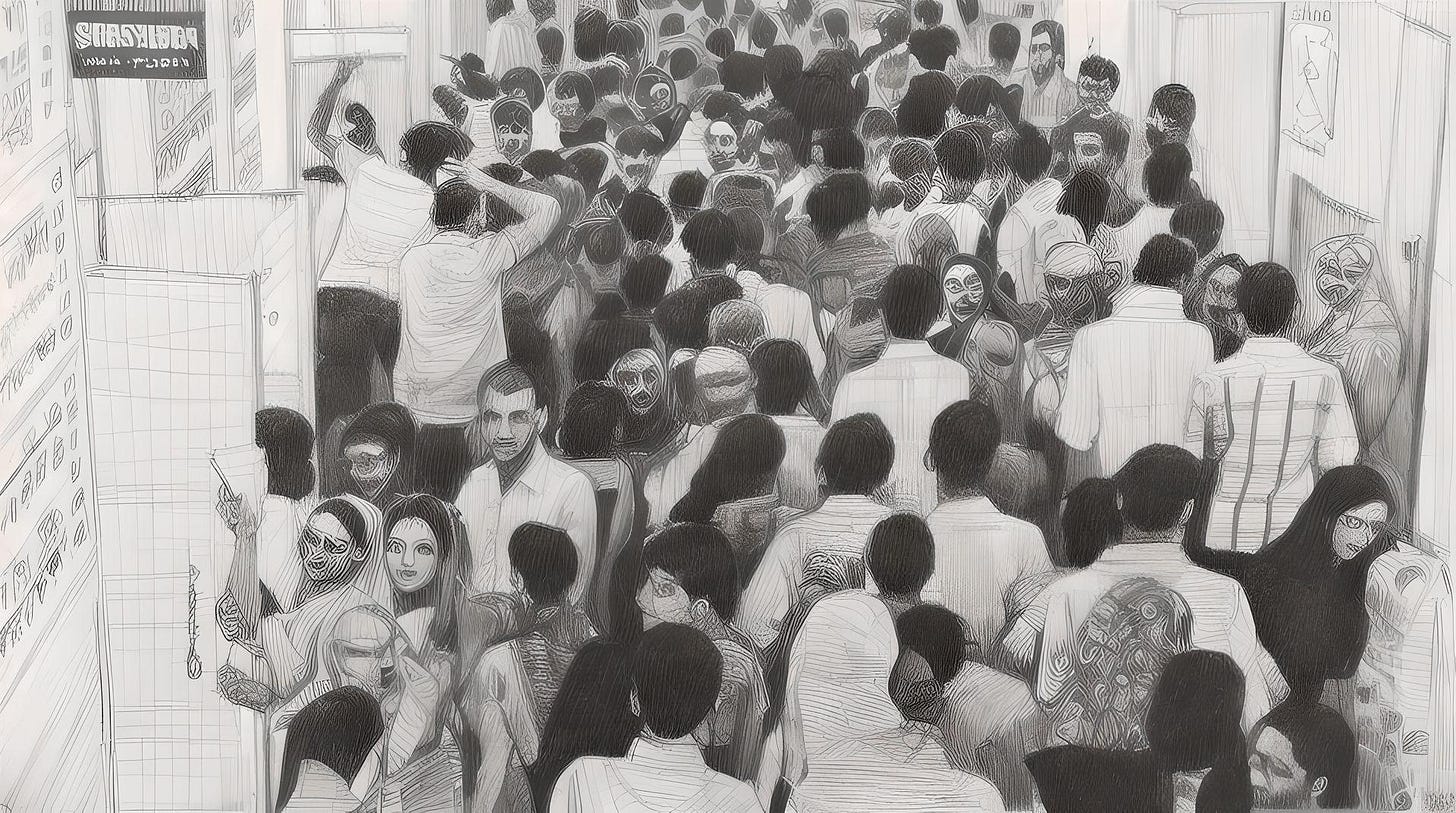
Now, lets flip the coin. When I enter a government hospital on a busy day(typically Monday to Wednesday) the reality hits hard. Its a huge hospital with multiple buildings and blocks, but narrow corridors are dark and overcrowded with patients. There’s no space to walk, long lines to get the OP slip, long lines of sick patients standing infront of consultation rooms with no proper waiting areas nor seating arrangements for patients. Everything appears free in a government hospital—until you're prescribed a test that can't be conducted there or medicines that aren't available in its pharmacy.
Waiting in long lines to give sample at diagnostic block. Simple tests like CBP, LFT, and CUE take a whopping 3 days for test results. The radiology block(Xray, Ultrasound, CT, MRI) is always overcrowded. when it comes to consultations, 3-4 doctors are often handling multiple patients in a single room, with no privacy—patients stand right behind one another, waiting for their turn. Doctors are overworked, consulting while performing tests, trying to meet the overwhelming demand. There are long walks from one department to another.
At government hospitals admissions into wards are quick, the emergency department operates 24/7, and healthcare here is accessible and affordable to everyone, but we can’t always count on reliability. A government self-assessment survey revealed that only 20% of public health facilities meet essential standards, with 42% scoring below 50%.(4)
Systemic Issues: The Root of Government Hospital Problems
This isn’t about glorifying or condemning any healthcare sector — this is the reality of what many of us experience at these hospitals. People — like you and me — are so acclimatised to the notion that government hospitals provide a relatively low quality healthcare, we don’t even care to demand for better quality of healthcare at government hospitals.
We are so acclimatised to subpar care, we forget to demand better.
We need policy changes, better infrastructure, and adoption of evolving technology in medicine to achieve a better healthcare for all. The government holds the sole responsibility to provide these facilities. I wouldn't mind if the Indian government taxed me specifically to fund healthcare development—similar to the FICA system in the United States. But this would not be necessary if Health Budget is allotted and utilised properly by the Government of India. Despite the allocation of substantial funds under various schemes, like National Fund for Persons with Disabilities (PwDs), a significant portion remains underutilised each year by the Government of India pointing to systemic inefficiencies in implementation, poor inter-departmental coordination, and limited outreach.
Electronic Medical Records : A Solution
The medical records of patients are digitalised and the entire history, previous prescriptions to medical tests data of each patient are one click away.Real-time access to test results, from basic blood tests to advanced 3D scans (CT, MRI), helps doctors make immediate decisions, especially in emergencies. When test results take time, doctors can still make provisional diagnoses. As the entire medical history is accessible via EMR systems, keeping track of treatment regimen and past illnesses or major health incidents becomes easier.
In India’s government hospitals,EMR systems are almost nonexistent. It can take three days for simple test results in OPD, due to an overwhelming patient inflow and understaffed diagnostic departments.There are no connected systems for doctors to share reports seamlessly. In fact, many doctors still take photos of important test results with their phones and share them via messaging apps with the treating doctors team to keep track of patient’s treatment records. This practice blurs the line between personal and professional life for doctors and raises concerns about patient privacy.(5)
The adoption of EMRs in India is limited, especially in government hospitals. While approximately 35% of Indian hospitals have implemented EMR systems, the majority are large private hospitals in urban areas. Government hospitals and rural healthcare centers lag significantly in EMR adoption. Initiatives like the Ayushman Bharat Digital Mission (ABDM), National Digital Health Mission (NDHM), National Digital Health Blueprint, and e-Hospital Initiative aim to bridge this gap by promoting digital health records across the country.(6)
Establishment of well connected Network of EMRs need a hefty initial investment, employing a whole new department to look after the EMR systems and training medical professionals(doctors to nurses) to opertae those EMR systems. A cybersecure EMR system would minimize the risk of privacy breaches.(5)
However, the reality in government hospitals is that technology is still in its infancy, and it is disorganized. In many Indian government hospitals, computers are primarily used for generating OPD appointment slips and for storing radiology scan images—far from realizing their full potential in healthcare delivery.
Patient Management
In quaternary hospitals, you need an appointment for everything—consultations, specialized tests, and surgeries. Though patient inflow is well-managed, the appointment system makes it difficult to get a consultation without prior scheduling. Once you have an appointment, however, the treatment process is relatively fast.
In contrast, every department is overcrowded in government hospitals. Patient inflow is so large, it leads to sick patients—often weak and vulnerable— standing in lines for hours to see a doctors in general medicine OPD. Then they have to get their tests done, wait for reports(often 3 days) and then again stand in line to get those reports reviewed. Some specialized tests, like Doppler ultrasound, are only available on specific days, and if you're unlucky, you might have to wait an entire week.
The Doctor–Population Ratio and Rural Health Access
With increasing MBBS seats in India, people talk about how, in comming years, doctors would endup like the surplus of unemployed engineering graduatutes. According to WHO guidelines India has achieved the target of a 1:1000 doctor-to-population ratio, standing at 1:811 in 2025 but urban–rural disparity persist. The problem lies in distribution. Most doctors are in urban cities, leaving rural areas severely underserved. States like Bihar and Uttar Pradesh have ratios worse than 1:2000. How can we tackle this distribution disparity problem? This remains a big hurdle as long as doctors find working in urban areas lucrative than working in rural areas. Solving this problem can be the next startup idea.(7,8)
The real crisis isn’t doctor count—it’s where they are.
The Role of NGOs and Policy Change
Numerous NGOs and Public Health volunteers are trying to solve this inequity to healthcare problem and trying to improve accessibility to healthcare in rural areas. While they play a crucial role, the core problem of unequal healthcare distribution can only be solved by government policy changes and a commitment to healthcare development. NGOs and volunteers may be a temporary band aid, but they cannot sustain systemic change in the long run.
The government must lead the charge, not just in fund allocation but also in ensuring that those funds are spent effectively. Healthcare should never be treated purely as a profitable business—it is a basic human right.
Precision Care Grid - A solution
A healthcare model that replaces the rigid, tiered Primary–Secondary–Tertiary system with a flattened, function-based network of Care Hubs, Satellites, and Mobile Units. It emphasizes universal EMR connectivity, AI-driven diagnostics and triage, and task-shifting to reduce doctor bottlenecks. By decentralizing services and enabling real-time data sharing, this system ensures faster, more equitable access to care across geographies. Emergency response is automated through predictive logistics, while mobile diagnostics and drone delivery expand reach. Funded by a dedicated healthcare tax, this model can transform healthcare into an adaptive, technology-driven public infrastructure.
From hierarchical tiers to nodes—let’s flatten the system, not patients.
This idea was brainstormed with the help of generative AI tools. This emphasises how AI can be integrated into planning to comeup with objective and ideal solutions.
Conclusion
In conclusion, the stark contrast between India’s quaternary care hospitals and government hospitals is not just a matter of infrastructure or funding—it reflects deeper systemic inequities in healthcare delivery, resource allocation, and governance. While quaternary hospitals represent the pinnacle of modern medicine, they remain inaccessible to most. Meanwhile, government hospitals, though more inclusive, struggle under the weight of inadequate infrastructure, staff shortages, and technological gaps. Bridging this divide requires not just investment, but a paradigm shift in how we view public healthcare—one that prioritizes accessibility, efficiency, and dignity for all patients, regardless of their income or location.
References:
Levels of Medical Care: Primary, Secondary, Tertiary, and Quaternary | VeryWellHealth
kauvery quaternary care hospital | KauveryHospital
Andhra Pradesh: Ramesh Hospitals to start quaternary care hospital at Amaravati | TimesOfIndia
India's healthcare in critical condition: 4 out of 5 public health centers below par, reveals new Govt report | EconomicTimes
EMR Adoption in India: Why Clinics Are Struggling to Keep Up | Linkedin
Electronic Medical Records in India: Current State, Challenges, and Future Prospects | LogicLoom
Will India's 10,000 New Medical Seats Solve the Doctor Shortage Crisis? | TimesOfIndia
Bridging the urban-rural divide | ExpressHealthCare
3 months for a test at Lok Nayak OPD, 45 days at Indira Gandhi hospital: Report in Delhi HC flags backlog | IndianExpress





0 Comments